Research Review: The Impact of Physician Empathy on Chronic Pain Management
A recent study underscores the crucial role of physician empathy in improving outcomes for patients with chronic low back pain, highlighting its significance over traditional treatments and even surgical interventions.
In pain management, especially for chronic conditions, the therapeutic relationship between physician and patient is pivotal. A recent study investigates how physician empathy correlates directly with better patient outcomes in chronic low back pain, providing a compelling argument for nurturing empathetic practices within clinical settings; I review the key points below.
Study Design & Methodology
The research, "Physician Empathy and Chronic Pain Outcomes," examined 1470 adults with chronic low back pain over the period from April 1, 2016, to July 25, 2023. Using the Pain Registry for Epidemiological, Clinical, and Interventional Studies and Innovation, the study assessed the impact of physician empathy on pain management, functional ability, and health-related quality of life (HRQOL). Empathy levels were measured using the Consultation and Relational Empathy (CARE) measure, categorizing physicians as either very empathic or slightly empathic.
Empathy Assessment and Patient Outcomes
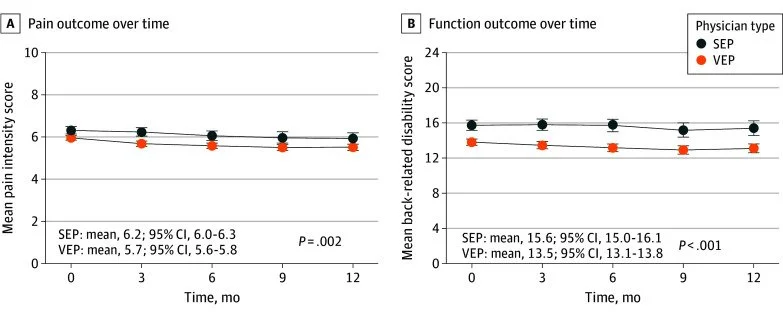
Patients reported their pain intensity, back-related disability, and HRQOL through standardized instruments like the Roland-Morris Disability Questionnaire and the Patient-Reported Outcomes Measurement Information System. The findings were clear: those treated by highly empathic physicians experienced significant reductions in pain and disability and showed improvements in various HRQOL measures, including anxiety, depression, and sleep disturbances.
The effectiveness of physician empathy was more pronounced than other treatments analyzed in the study. Patients treated by very empathic physicians reported significantly better outcomes than those treated by slightly empathic physicians, with differences that were not only statistically significant but also clinically relevant:
Pain Intensity: The study revealed that patients in the very empathic physician group reported lower mean pain intensity scores compared to those in the slightly empathic group (6.3 vs 6.7 on a scale of 10, p < .001). This reflects a marked reduction in perceived pain levels.
Back-Related Disability: Similar trends were observed for back-related disability, where patients treated by more empathic physicians reported lower disability scores (14.9 vs 16.8 on the Roland-Morris Disability Questionnaire, p < .001), indicating better functional outcomes.
Health-Related Quality of Life (HRQOL): Across various HRQOL measures, including fatigue, sleep disturbances, and pain interference, the very empathic physician group consistently reported fewer deficits. For example, in the fatigue measure, scores were 57.3 for the more empathic group versus 60.4 for the less empathic group, demonstrating a significant improvement (p < .001).
Diagram via PMID: 38602675
Comparative Analysis of Physician Empathy to Other Pain Management Options
Notably, the effectiveness of physician empathy outshined other treatments such as nonpharmacological therapies, opioid prescriptions, and even lumbar spine surgeries. This underscores the profound impact that empathetic patient care can have, surpassing even the more invasive and conventional medical interventions.
Here is a detailed list of relevant statistics from the study comparing physician empathy to other medical interventions:
Pain Intensity Comparison:
Very Empathic Physician Group: Mean pain intensity = 6.3
Slightly Empathic Physician Group: Mean pain intensity = 6.7
Statistical significance: p < .001
Clinical relevance (Cohen's d): 0.21
Back-Related Disability Comparison:
Very Empathic Physician Group: Mean back-related disability = 14.9
Slightly Empathic Physician Group: Mean back-related disability = 16.8
Statistical significance: p < .001
Clinical relevance (Cohen's d): 0.30
Health-Related Quality of Life (HRQOL) Comparison - Fatigue:
Very Empathic Group: 57.3
Slightly Empathic Group: 60.4
Statistical significance: p < .001
Clinical relevance (Cohen's d): 0.30
Health-Related Quality of Life (HRQOL) Comparison - Sleep Disturbance:
Very Empathic Group: 56.6
Slightly Empathic Group: 59.1
Statistical significance: p < .001
Clinical relevance (Cohen's d): 0.28
Comparison to Nonpharmacological Treatments, Opioid Therapy, and Lumbar Spine Surgery:
Opioid Therapy: Associated with greater pain intensity and disability compared to those not on opioids.
Lumbar Spine Surgery: Associated with greater back-related disability compared to those without surgery.
The Role of Empathy in Clinical Practice
The study sheds light on the power of empathy in medical practice, suggesting that a physician's ability to empathize can lead to better patient adherence, enhanced treatment outcomes, and overall satisfaction. This relational dynamic is particularly critical in managing conditions like chronic pain, where emotional and psychological factors significantly intersect with physical health.
Encouraging a culture of empathy within healthcare settings could transform patient experiences and outcomes. Physician empathy emerges not just as a beneficial but an essential component of effective clinical practice, particularly in the field of pain management. As healthcare continues to evolve, integrating empathy into patient care protocols could be revolutionary, promising not only to improve clinical outcomes but also to enhance the quality of life for patients with chronic conditions.
Read the full study here.