Research Review: Is Off-Label Repeat Prescription of Ketamine as a Rapid Antidepressant Safe?
Dr. Weiner reviews a recently published deep dive into ketamine's use as a rapid antidepressant, exploring its potential and pitfalls and highlighting therapeutic effects, ethical concerns, and safety issues in treatment-resistant depression.
Recent discussions surrounding the use of ketamine as a rapid antidepressant, particularly in cases of treatment-resistant depression, have drawn attention due to its controversial use and potential for abuse. A recent research review explores the use of off-label ketamine prescriptions, emphasizing the necessity for stringent safety measures, ethical considerations, and robust clinical evidence to support its use
Below, Dr. Weiner reviews the key points of the research and then provides feedback on the concerns raised and reviewed.
Key Point 1: Ketamine’s Role and Effects as an Antidepressant
Ketamine, traditionally used as an anesthetic, has shown promise in rapidly alleviating depressive symptoms. Clinical trials suggest that even sub-anesthetic doses of ketamine can lead to quick improvements in mood. However, these effects are often short-lived, with a significant risk of relapse within days after treatment. This temporary relief poses ethical questions about the feasibility and safety of repeated ketamine infusions, especially given its addictive potential and severe side effects, including cognitive impairment and urinary tract issues.
Key Point 2: Clinical Trials and Off-Label Use
Many clinical trials investigating ketamine's antidepressant properties have limitations, including small sample sizes and short follow-up periods. These factors hinder the generalizability of results and raise concerns about the long-term safety of ketamine therapy. Despite FDA approval for its use as an anesthetic, ketamine's application in treating depression remains off-label. This status requires clinicians to tread carefully, balancing rapid antidepressant effects against potential abuse and ethical dilemmas.
Key Point 3: The Controversy of Repeat Prescriptions
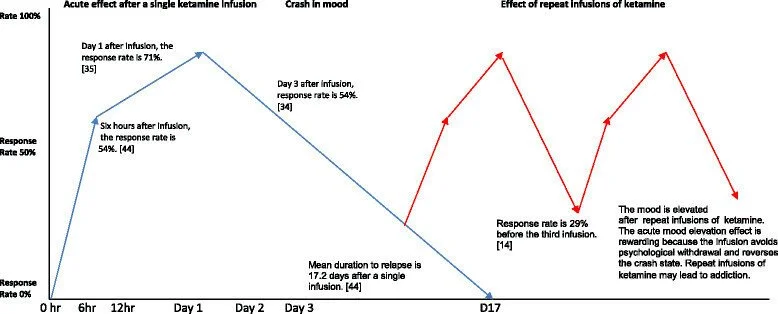
The debate intensifies when considering repeat prescriptions of ketamine. The graph included in the study illustrates a significant drop in response rates after initial treatments and the diminishing returns with subsequent doses (see attached diagram). This pattern highlights the complex nature of ketamine's efficacy and underscores the risks of dependency and tolerance that can arise from multiple infusions.
Key Point 4: Ethical and Legal Implications
The researchers posit that administering ketamine off-label for depression navigates a murky ethical landscape. It challenges the principles of autonomy by potentially influencing patient decision-making under distress and breaches nonmaleficence due to adverse side effects. The legal ramifications are equally daunting, as the drug’s potential for abuse places significant responsibility on prescribing physicians to ensure that the benefits outweigh the risks.
Case Studies Highlighting Ethical Concerns
Two case vignettes provided in the study shed light on the ethical complexities involved in prescribing ketamine. The first case illustrates a scenario where ketamine is chosen over more conventional treatments like ECT, raising issues of fidelity and informed consent. The second case involves a patient with a history of substance abuse, highlighting the risks of recurrence and legal issues that can ensue from such prescriptions.
Diagram via PMID 26768892
Dr. Weiner’s Feedback:
While the potential of ketamine in treating depression, anxiety, and mood disorders quickly is undeniable, its high addiction risk, particularly with take-home forms like nasal sprays and recreational use, remains a significant concern. This is why I advocate for administering ketamine via intramuscular (IM) or intravenous (IV) routes, under controlled clinical conditions. It is also crucial that this treatment is not viewed as a standalone solution.
Comprehensive support through coaching or therapy is essential, ensuring that every patient engages in both preparatory and integrative practices. This holistic approach not only mitigates risks but also enhances the therapeutic outcomes, leveraging the benefits of ketamine while safeguarding against its pitfalls.
The graph provided in the study of response rates (to my knowledge) is measuring strictly ketamine, without coaching or therapy - I believe that ketamine is not a quick-fix; it is simply a tool to be utilized in the process of “reprogramming” our highly neuroplastic minds. While the window of high opportunity for change is relatively narrow (approximately 24 hours), if proper integration practices are implemented, the outcomes can be truly life-changing, and at the very least, life-improving.
Implications for Ketamine in Medical Practices
While ketamine presents a novel treatment pathway for those suffering from severe depression, its use is fraught with challenges that require careful consideration of ethical, legal, and clinical factors. Clinicians must be diligent in evaluating each case, ensuring comprehensive patient education about risks and maintaining rigorous monitoring to mitigate potential abuse.
The call for a balanced approach to ketamine use in depression treatment is clear. As research progresses, the medical community must remain vigilant about the rapid developments in ketamine therapy and continuously update practices to safeguard patient welfare. Only through concerted efforts can the potential benefits of ketamine be harnessed responsibly, ensuring that its application in clinical settings adheres to the highest standards of medical ethics and patient care.